Vitiligo
What is vitiligo?
- Vitiligo is a long-term skin condition caused by the loss of melanocytes, the cells responsible for producing melanin which gives colour to hair, skin and eyes.
- It is an autoimmune disorder where the immune system mistakenly attacks and destroys the melanocytes.
- It is not contagious or life-threatening but can significantly impact self-esteem.
- Famous people with vitiligo include Michael Jackson, late singer and pop icon; and Jon Hamm, famous for his role as John Draper from “Mad Men”.
- Hamm says his vitiligo was worsened by the stress of filming.

What are the symptoms of vitiligo?
- Depigmentation, or the loss of pigment in the skin on various parts of the body, resulting in white or light patches.
These patches have a characteristic chalk or milky-white appearance. - Premature whitening of hair, early graying or whitening of hair on the scalp, eyebrows, eyelashes or beard.
Sometimes vitiligo can cause loss of colour in the mucous membranes of the mouth, nose and genitals, which may get lighter or turn white. - The lesions are typically asymptomatic but rarely pruritic.
- The lesions may be well defined with the borders sometimes either the colour of the unaffected skin, or inflamed and red.
- Sometimes smaller patches merge.
- Vitiligo can often have a significant psychological impact on mood and self-esteem.
Does sunlight make vitiligo worse?
- Yes sunburn may trigger vitiligo.
- Sunburn and sun sensitivity ongoing as the depigmented patches have a reduced ability to protect skin from sun damage.
- Sun exposure and damage from UV rays can also make skin prone to burning and tanning makes discoloured areas look more prominent.
What causes vitiligo?
- Genetics is heavily implicated, however it’s thought the condition is a complex matrix of genes, immunological, biochemical, oxidative and environmental mechanisms at play – this is known as “integrated theory”.
- Vitiligo can also be exacerbated by injury such as burns, cuts, lip-licking or eye-rubbing or even tight fitting clothes.
Who gets vitiligo?
- Genetics is heavily implicated, however it’s thought the condition is a complex matrix of genes, immunological, biochemical, oxidative and environmental mechanisms at play – this is known as “integrated theory”.
- Vitiligo can also be exacerbated by injury such as burns, cuts, lip-licking or eye-rubbing or even tight fitting clothes.
What causes vitiligo?
- Genetics is heavily implicated, however it’s thought the condition is a complex matrix of genes, immunological, biochemical, oxidative and environmental mechanisms at play – this is known as “integrated theory”.
- Vitiligo can also be exacerbated by injury such as burns, cuts, lip-licking or eye-rubbing or even tight fitting clothes.
Who gets vitiligo?
- Men and women are equally impacted but women tend to make up a greater percentage of vitiligo doctor visits due to concern with cosmetic appearance.
- The average onset is age 20-24 but it can occur at any age.
- Typically there are two onset peaks (below 10 years of age) or later after age 30.
- The overwhelming majority (about 80%) of all cases present before the age of 30.
- Vitiligo is more common in patients with naturally dark skin.
- People with vitiligo have higher chance of thyroid disease.
- Less frequently, people with other autoimmune conditions such as rheumatoid arthritis, insulin-dependent diabetes, psoriasis, lichen sclerosus, pernicious aneamia, Addison Disease and alopecia areata are affected by vitiligo.
- Vitiligo is also 3x more common in bone marrow and stem-cell transplant recipients than in the healthy population.
What are the different types of vitiligo
– Universal vitiligo is when the discoloration affects almost all of the skin surface.
– Generalised vitiligo is when the pigmented patches progress symmetrically on corresponding body parts.
– Segmental vitiligo is when the patches occur only on one part or on one side of the body and this tends to be more prevalent in young people, progresses for a couple of years and then stops.
– Acrofacial vitiligo affects the face and hands, eyes, nose and ears.
How is vitiligo diagnosed?
The diagnosis of vitiligo generally requires Dr Parisa taking a medical history, examining your skin with a special lamp, and skin biopsy and blood tests.
What is the treatment for vitiligo?
No single medication can stop vitiligo. However some drugs used alone or in combination with light therapy can help restore colour. Treatments include:
- Topical corticosteroids that control inflammation when vitiligo is in its early stages, and may help skin return colour. Side effects may include skin thinning or lines or streaks on skin.
- Topical calcineurin inhibitors such as tacrolimus and pimecrolimus may help small white patches of the face and neck.
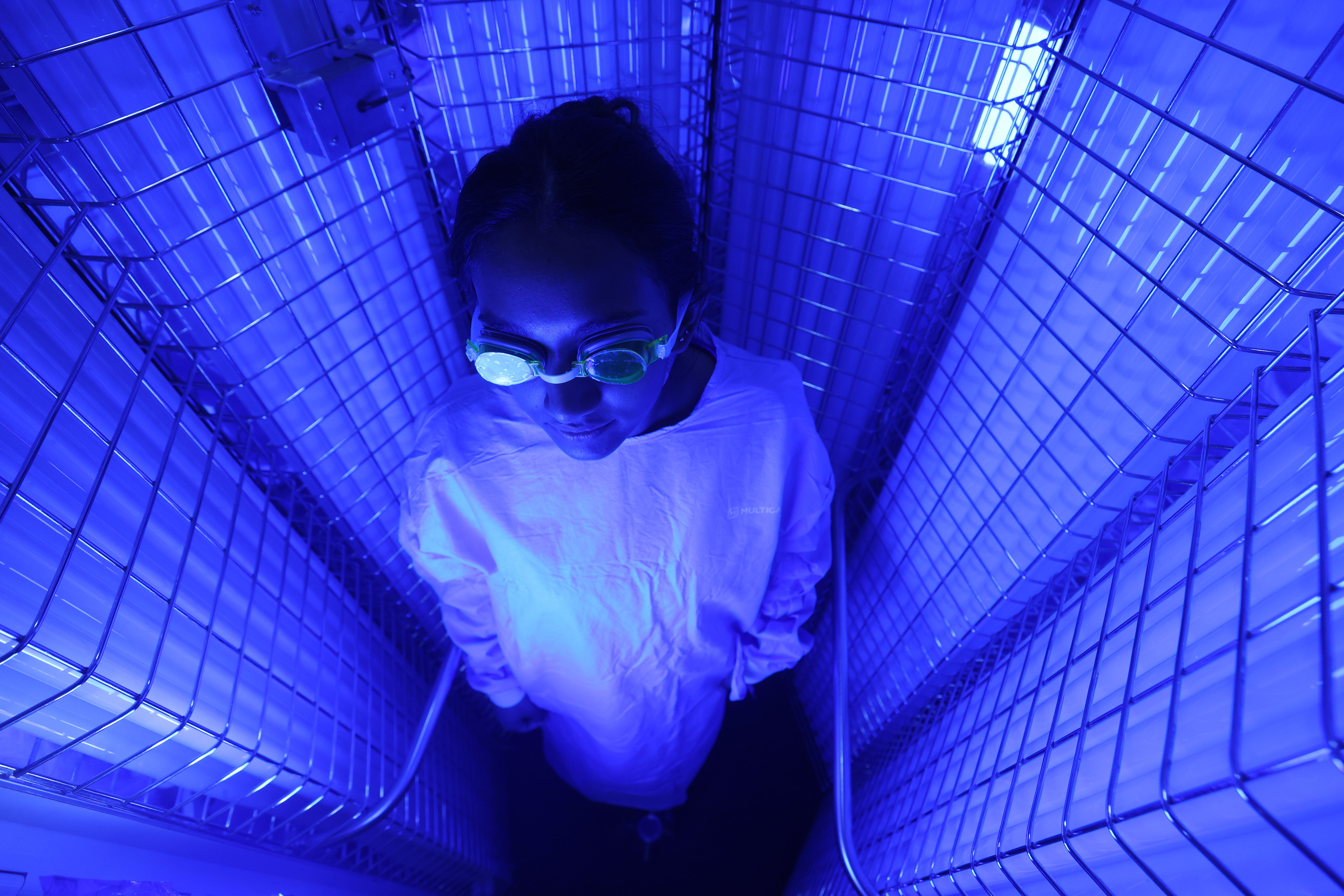
- Phototherapy (Narrowband UVB) which we bulk-bill in our clinic can be effective to control progression especially when used with corticosteroids or calcineurin inhibitors. This needs commitment and involves coming to rooms three times a week for 3-6 months. See more about phototherapy here.
- Biologic medications such as Jak inhibitor Opzelura (Ruxolitinib)is a topical Janus kinase (JAK) inhibitor currently approved for vitiligo treatment.
- Immunsuppresant medication such as methotrexate ,cyclosporine,azathioprine.
- Surgical Procedures such as skin grafting where a surgeon transfers small sections of health skin to white areas. This is generally only effective for small patches of vitiligo.
Cosmetic Camouflage – Ask us about vitiligo camouflauge makeup to cover vitiligo spots.
How long does vitiligo last?
Vitiligo can occur over a few months, then stabilizes.
Some spontaneous repigmentation may occur from hair follicles and the overall size of the white patch will reduce.
However in most cases, vitiligo tends to extend again and the areas of pigmentation increase with time.
Cycles of pigment loss, followed by periods of stability are typical and can occur indefinitely.
How can I improve my quality of life with vitiligo?
- Don’t get a tattoo which may cause patches within weeks.
- Use make-up to conceal affected skin or self-tanners that contain dihydroxyacetone which has colour and can camouflage
- Practice excellent sun protection using a broad-spectrum, water resistant sunscreen and reapply every two hours when swimming.
- Speak to your doctor or dermatologist regarding referrals to mental health providers (depression and self-esteem issues are common in people with vitiligo).
Did you know?
- People with vitiligo might have a lower risk for internal malignancies and skin cancer.
- Two nationwide retrospective studies from South Korea and Taiwan, have shown that vitiligo patients are at lower risk of internal malignancies, in addition to lower BCC and SCC.
- Another study found vitiligo patients are at lower risk for both melanoma and NMSC, however there may be a possible higher risk for thyroid cancer. ~ DermnetNZ